Project title
The structural and organisational impacts of perioperative enhanced care services in the UK: A Retrospective Evaluation of Post-operative Alternatives to Critical Care (REPACC)
Country
UK
Background
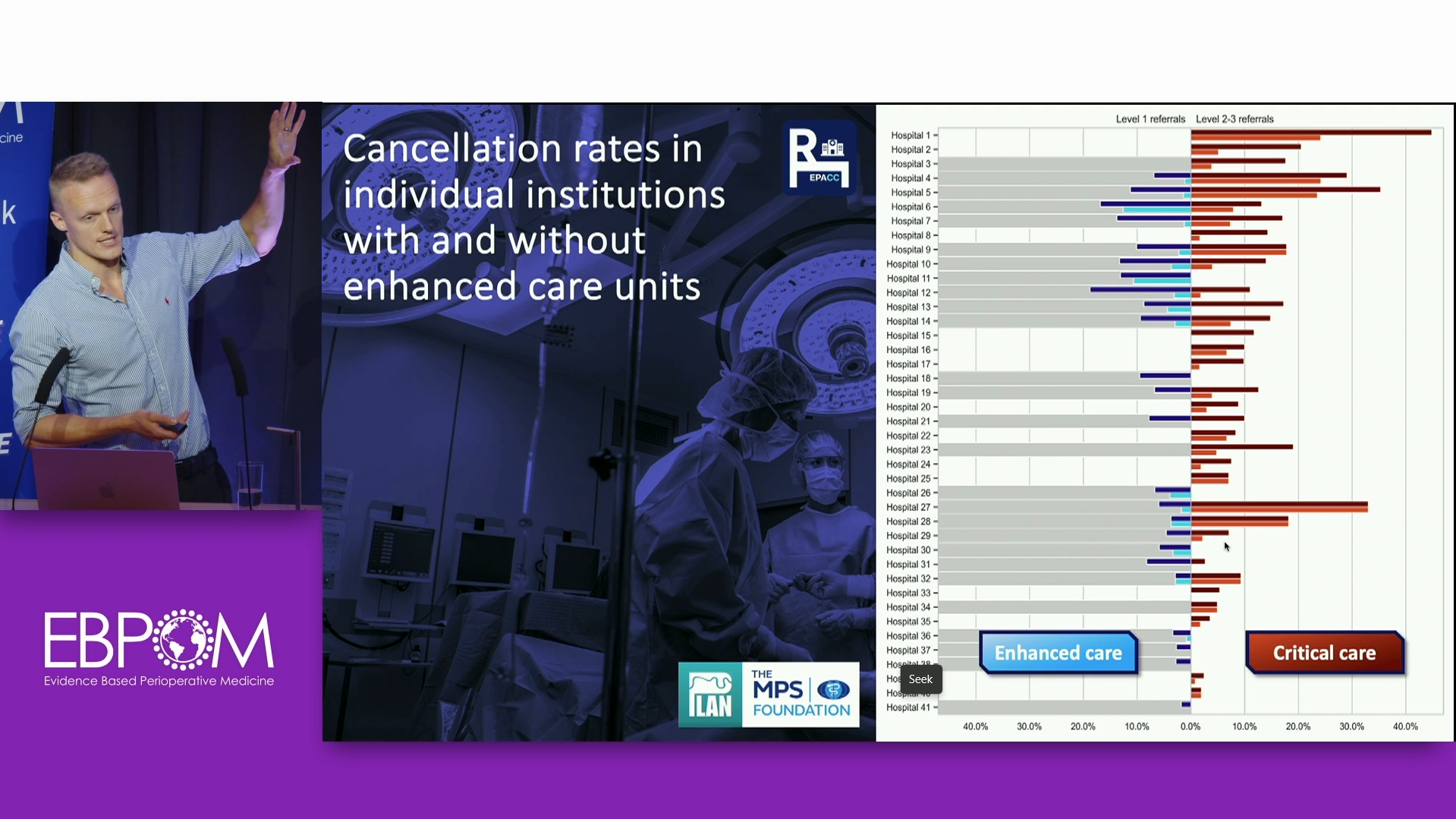
Delivery of post-operative critical care for high-risk surgical patients represents a significant challenge within the NHS, due in part to high bed occupancy rates, with general and acute bed occupancy increasing exponentially. As a result, rates of on-the-day cancellation of elective surgical procedures for non-clinical reasons are at unprecedented levels, leading to delays to definitive care which is associated with potentially life altering consequences for service users.
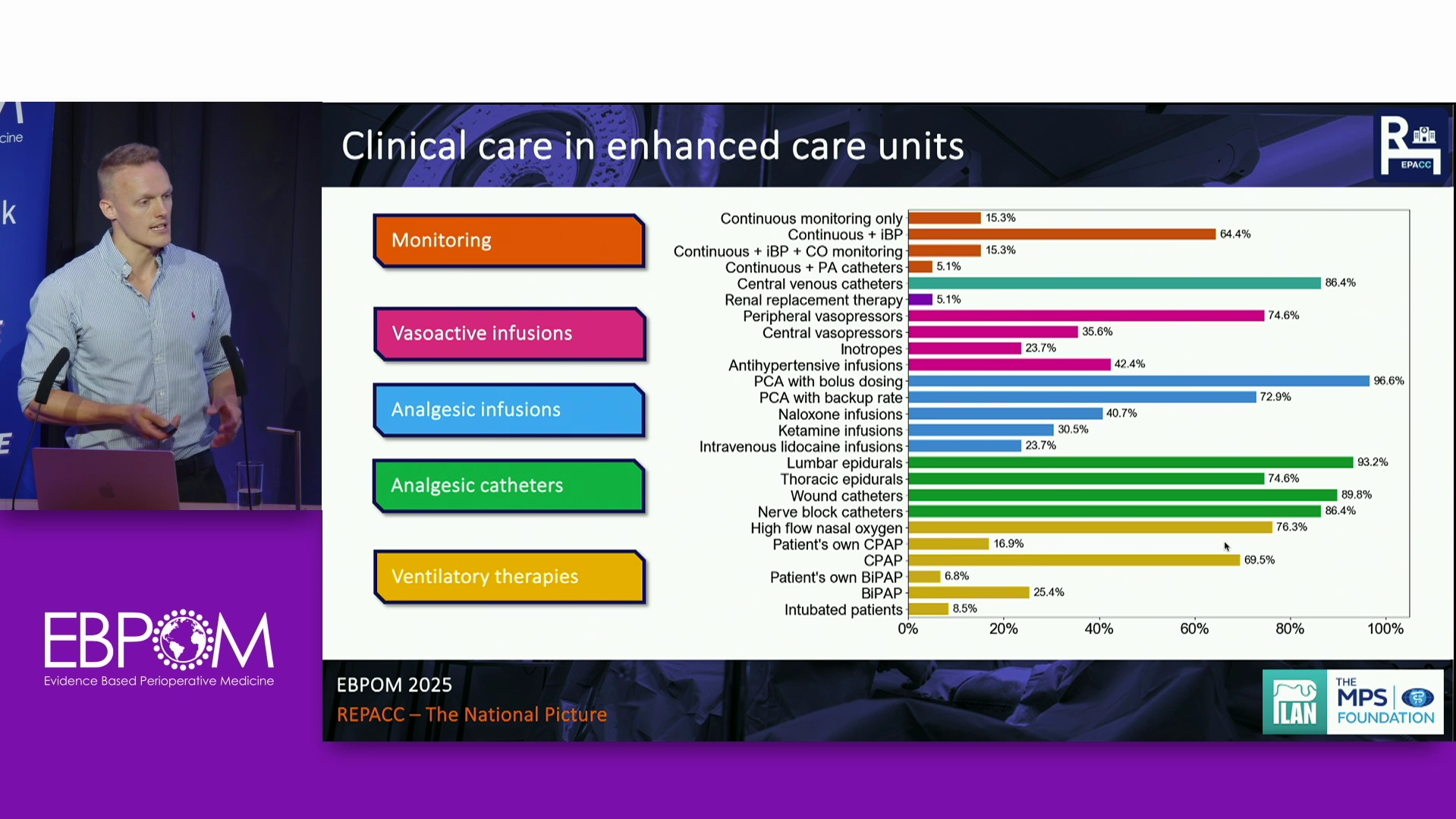
The requirement for a post-operative critical care bed is independently predictive of on-the-day cancellation of elective surgery. Thus, to reduce unnecessary cancellations, and their associated morbidity, new models of care such as Post-Anaesthetic Care (PACU) and Overnight Intensive Recovery (OIR) units have evolved. While these models of care are there to improve organisational efficiency, there is speculation that reduced clinical and risk score thresholds for admission to them may end up increasing the likelihood of on-the-day cancellation if these services are over-burdened. Furthermore, there is concern that the resources available, clinical oversight, and staff training within enhanced care units may not be adequate to care for high-risk patients that would traditionally be admitted to intensive care.
There is a paucity of independent literature addressing the organisational impacts these models of care can have. It is also yet to be established whether these units achieve their objectives of improving patient flow, reducing pressure on intensive care, preventing on-the-day cancellations, reducing costs, and improving clinical outcomes in intermediate-risk surgical patients. Policy makers therefore have little to guide them in the development of these new models of care, thus exposing patients to an uncertain degree of risk.
Summary
REPACC is a multicentre retrospective cohort study investigating the provision and delivery of enhanced care, a model of care that lies somewhere between high-dependency units (HDU) and normal wards, such as overnight intensive recovery and post anaesthetic care units (OIR and PACU). The hope is to use this data to make enhanced care services more efficient, reduce pressure on critical care beds, and prevent unnecessary surgical cancellations.
The study will consist of two main components:
1. A qualitative appraisal of the structure of enhanced care services at participating centres.
2. A retrospective analysis of on-the-day cancellation rates, and several other measures of organisational efficiency, in patients referred to enhanced care facilities for post-operative care between a specified period.
Outcome
The outcomes of this project will be to address the evidence gap and improve the current knowledge available on these models of care. We also anticipate positive impacts for organisations and patients through improvements in the efficiency and safety of perioperative care services. Better designed enhanced care services, informed by the recommendations from this study, may improve patient flow and the resilience of these systems to variable demand, and reduce rates of on-the-day cancellation, which would not only be desirable but would reduce the morbidity associated with delaying definitive treatment.
Longer term, the findings from the study could facilitate the process of formulating national and international guidelines to guide policy makers responsible for the development of these services.
Dr Chris Oddy recently presented the findings of the study at the recent 2025 EBPOM Conference:
The findings of the project have been published:
Population characteristics of individual enhanced facilities in the UK compared with critical care

